91 Americans lose their lives every day to opioid overdose, according to the Centers for Disease Control and Prevention (CDC). That is over 33,000 Americans each year, and the rate is only rising, actually having quadrupled since 1999. It is now accurately categorized as an Epidemic and, appropriately, stringent private and public institutional changes are being implemented to minimize the likelihood of future abuse. This includes limited pill counts, prescription drug monitoring platforms, closed formularies, etc. These improvements reduce the likelihood of future dependency, but what about those already dependent, the most at risk for potential overdoses. What can we do about them?
The first answer: Keep them alive. Enter the growing availability of Opioid Rescue Therapies. Two of the most commonly prescribed are Narcan® and Evzio®. Both medications utilize naloxone, an opioid antagonist, which can be a life-saving treatment in the case of an opioid overdose. Rescue Therapies have become standard issue to police, emergency medical personnel, and recently have become available over-the-counter without a prescription at participating CVS Pharmacy® locations in 41 states. The reason: they work.
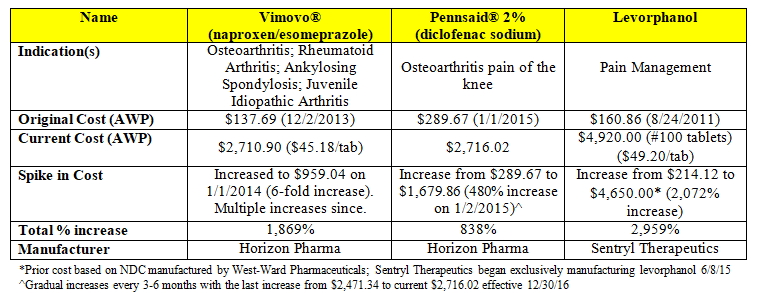
However, we cannot have Rescue Therapy serve as just a ‘Band-Aid’. Furthermore, the issues of cost need to be addressed. There are currently multiple formulations of naloxone available, the cost of which varies dramatically. Evzio® ($4,500.00) is a brand-name naloxone auto-injector that uses a pre-filled device with a voice-prompt providing direction for use. Conversely, Narcan® ($150.00) is a fast-action nasal spray that also provides two doses, but at a fraction of the cost.
Prescribing naloxone should be viewed as one step in a comprehensive opioid risk assessment strategy. Patients, prescribers, and loved ones should periodically question the opioid doses/regimen employed. Is it effectively reducing pain and improving function with minimal side-effects? Could a lower dose provide similar efficacy with a reduced overdose risk? Has weaning been tried recently? Has an opioid rotation to a lower dose alternative or non-opioid pain reliever been trialed?
When further examining treatment, it is also important to consider additional risk factors, such as other medications employed and co-morbidities. For example, patients with COPD or sleep apnea or who are prescribed opioids in conjunction with central nervous system (CNS) depressants such as diazepam or clonazepam are at a significantly increased risk for overdose.
While the decision to prescribe naloxone can be a necessary emergency step, it is important it be viewed as a window of opportunity for patients and prescribers alike to address the current medication regimen, while ensuring the most cost-effective naloxone formulation is easily accessible for the patients who need it most.
About the Author: Anthony Sambucini is a founding principal and the Chief Executive Officer of ANS Solutions. Anthony specializes in bridging the goals of clinical innovation and business strategy that have helped propel ANS Solutions into a national leader in Pharmacotherapy Review Services for workers’ comp insurers and ANS Pharmacotherapy Review Program is the most advanced, results-oriented drug utilization review program in the industry. As a consultant to insurance carriers and attorneys, Anthony customizes services based on the particular needs of the client and oversees all activities related to business development and company operations. For more information about ANS Solutions visit http://ans-solutions.com/.
Original content posted on http://ans-solutions.com/opioid-rescue-therapy-not-just-quick-fix/